Implementing digital health to transform primary health care in LMICs
In 2021, McKinsey & Company partnered with Exemplars in Global Health to research the success factors that can drive effective, widescale implementation of digital tools across health care systems in LMICs. The findings resulted in potential pathways to drive the implementation of digital health care in a manner that has the potential to transform primary health.
Read the full paper here: Unlocking digital healthcare in lower- and middle-income countries.
The COVID-19 pandemic has both highlighted and exacerbated the gaps in access to health care around the world, but particularly in lower- and middle-income countries (LMICs). Prior to the pandemic, almost a third of the population in LMICs already lived more than two hours away from essential health services, and the ratio of health care workers to population was typically well below the minimum recommended by the World Health Organization. But in the last year, the loss of health care workers to COVID-19 and the disruption of transport systems due to lockdowns have likely made that access – or lack thereof – even worse.
However, during this difficult time, a silver lining has surfaced to benefit those most in need: the growth in digital tools. Digital technologies, like those highlighted in Exemplars in Global Health case studies, have unmatched potential not only to improve countries’ responses to infectious diseases, but to strengthen their primary care systems. And with companies reporting an unprecedented acceleration in the adoption of digital technology, digital health tools used to address COVID-19 may pave the way for a transformation in primary health care systems well beyond the pandemic.
As with all things COVID-19, the world has seen firsthand that merely discovering a solution – like a vaccine – only begins to solve a problem. In the equation of Research, Development and Implementation (RD&I), implementation is often the most beleaguered of steps. For digital health tools, the very same applies. Merely discovering digital tools and technologies only begins to solve a problem. For them to be truly impactful, they must be enabled within a national health ecosystem that has effective national governance, sustainable financing, a strong regulatory environment, health data interoperability, digital readiness, and multi-sector engagement.
Click here to view larger image.
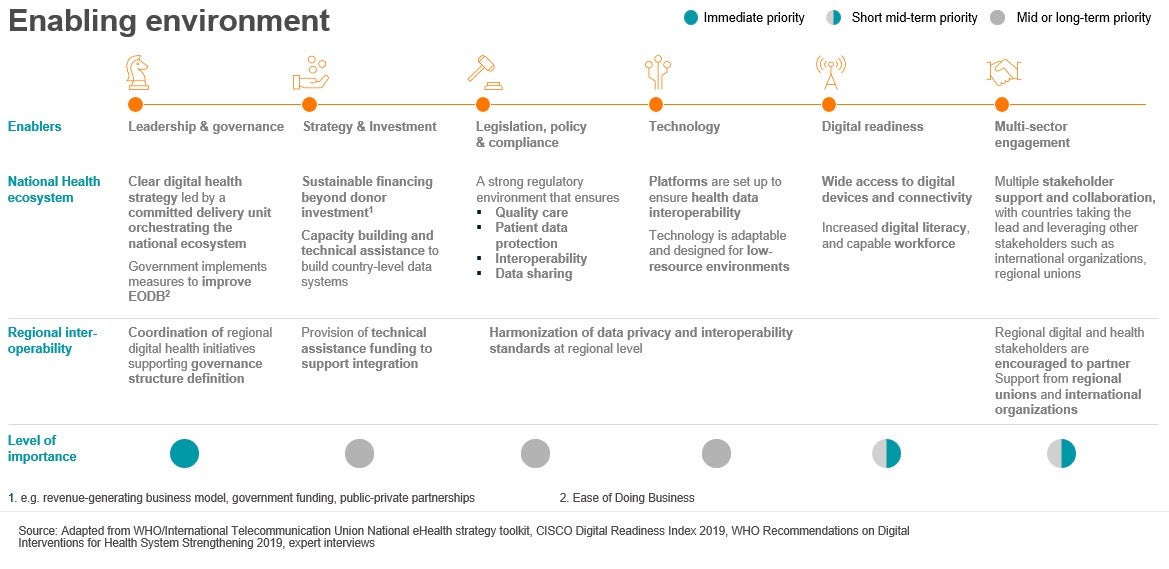
Of all of these, governance and digital readiness are the essential differentiators, if a country is to experience implementation success.
Countries with a government-led digital health effort and those with strong digital foundations tend to prioritize digital health strategies through data exchange and interoperability at national level. They also tend to intervene directly by creating dedicated teams responsible and accountable for implementing digital health strategies, ensuring capability building to support. And finally, they tend to develop mechanisms for sustainable financing of the digital health infrastructure, beyond donor funding.
Our research found that in Rwanda, a country that, thanks to its strong political will and partnerships, is becoming a digital health success story. Through its national growth strategy and its 90 percent universal health care coverage, the Rwandan government produced an environment that was ripe for improving its digital readiness. By ensuring over 90 percent of the population had access to broadband, Rwanda was then able to focus its digital capabilities on HCWs to scale telehealth, and the adoption of drone delivery for essential medical products.
We also saw this in India, where a flourishing digital health private sector, coupled with strong political will, has greatly contributed to a more powerful national health ecosystem. The country’s flourishing digital health start-up landscape is buoyed by investments (between 2014 and 2018, health-tech start-ups raised a total of US$504 million), and strengthened by the government’s commitments to improving a digital infrastructure that enables interoperability.
And in Ethiopia, we saw the country accelerate its digital journey, leapfrogging some of its LMIC peers, thanks to strong government leadership and co-creation and co-funding partnerships with donors. The country prioritized its digital health strategy, adopted best practices in IT, and fostered a culture of data use at all levels of the health system. It then invested in end-user training and created the Digital Health Innovation and Learning Center to foster innovation.
Implementation success can lead to expanded health care coverage, allowing broader reach of health care delivery through technological solutions. Whether it is through triaging at the right levels to ensure equitable care, or greater and faster patient access to health information, or more effective disease prevention and treatment, or using telemedicine for remote monitoring and diagnosis, well-implemented digital health tools can expand coverage for all.
Where there is a commitment to implementation, there tends to exist better quality of care. By supporting improved data sharing and analytics for evidence-based guidelines to improve outcomes, allowing health care workers to focus more time on patients, or even educating both through e-learning platforms, countries are improving the kind of care available to those who did not have it in the first place.
And finally, by enabling earlier risk-detection through predictive analytics and enabling long-term cost management, strong implementation can have a lasting impact on efficiency. By allowing increased division of labor and improved utilization through centralized, coordinated, real-time management of patients, supplies, and workflows, it can optimize resources, enabling lasting change.
If necessity is the mother of invention, this last year has generated enormous demand for innovative solutions that have saved lives. Through effective implementation of digital tools, many countries have paved the way for impactful innovations that will endure beyond COVID-19.
