COVID accelerating investments reshaping health supply chains
The pandemic disrupted supply chains around the world. In its wake, health leaders are doubling down on efforts to make their supply chains more resilient, sustainable, responsive, and equitable
COVID accelerating investments reshaping health supply chains
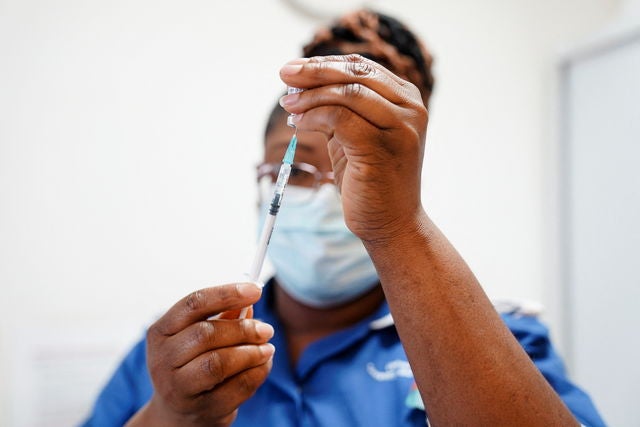
In Malawi, some patients were told to bring their own syringes to medical appointments. In Zambia, many women couldn’t access their preferred family planning method for months. And in Ethiopia hospitals experienced stock outs of first-line tuberculosis drugs. Each of these COVID-19 driven disruptions to public health supplies served as a painful illustration of the need for health systems to strengthen their supply chains.
The disruptions cost countless lives, led to an estimated 1.4 million unintended pregnancies globally in the first year of the pandemic alone, set childhood immunization services back years, and prompted health leaders like Dr. Sergio Artur Gomes, who leads distribution for Mozambique’s Central de Medicamentos e Artigos Medico, to prioritize strengthening their supply chains to make them more resilient, sustainable, responsive, and equitable.
Dr. Sergio is blunt about the pandemic’s impact on his country’s public health supply chain: “It showed our weaknesses.” And it doing so, he said, it provided some insights into how health leaders might do better.
Dr. Sergio and others in the field divide post-pandemic investments in rebuilding and strengthening public health supply chains into four broad categories. First, the pandemic opened the door to more robust engagements with the private sector. Second, it accelerated efforts to integrate the distribution of public health supplies. Third, it forced health leaders to realize that supply chains can't end at health facilities but must also connect with community health workers. Fourth, it opened governments to the pressing need for technology to monitor the delivery of services and supplies.
These new strategies and investments, especially in sub-Saharan Africa, offer health leaders seeking to improve their public health supply chains a variety of models to adapt and adopt. Some are a marked shift from previous approaches.
For example, governments have traditionally been very cautious about the role of the private sector in public health. The pandemic prompted many governments to rethink their stance.
The Democratic Republic of the Congo, for example, is now considering major changes involving the private sector. “Up until now, it was illegal for a public health facility to buy from private, for-profit pharma distributors,” said Joseph Roussel, director of private sector engagement at VillageReach. “The pandemic has created a heightened awareness of the need to increase options for supply and the DRC is expected to pass a presidential decree so that health facilities have additional options to the current supply system.”
Similarly, South Africa, Uganda, and Zimbabwe have launched efforts to leverage the private sector to help with the distribution of medicine. The countries have started pre-packaging commodities for HIV and chronic diseases for distribution to many patients through community distribution points and private pharmacies, taking the burden off public health facilities and reducing travel costs and time for patients.
Research by Médecins Sans Frontières and others find that such models have reduced workloads for overburdened public health providers, increased enrollment in health facility treatment programs, improved retention, reduced waiting times, and improved treatment access.
Meanwhile, Liberia’s health leaders also shifted their thinking about who the supply chain serves and what success looks like. In the country’s supply chain master plan written before the pandemic, health facilities were considered the end point of medical supply distribution – overlooking the thousands of community health workers (CHWs) who serve communities. Their work keeping communities safe and healthy during the pandemic prompted a rethink. Today, a revised master plan outlines how the country can integrate supplies for CHWs into the broader facility supply chains.
“COVID opened a strong channel of radical and robust collaboration between governments and CHW organizations,” said Tapiwa Mukwashi, Director of the Global Technical Team at VillageReach. This collaboration was led by a coalition of organizations working together, the COVID-19 Action Fund for Africa.
The pandemic prompted Mozambique’s leaders to accelerate investments and innovations to strengthen their public health supply chain across these four categories. For example, in 2015, Mozambique’s Ministry of Health began a pilot to test outsourcing of transportation of a small number of health supplies in a single province. By the time the pandemic hit, the country was in the process of scaling the program nationally and could see the impact play out across the country. “During COVID, we could see that the provinces using private sector transport had fewer stock outs,” said Esselina Brito, Outsourced Transport Advisor for VillageReach in Mozambique.
Other countries, including Ghana and South Africa, have done the same, with the Africa Resource Center developing a toolkit to guide health leaders through the outsourcing process.
As part of this process, Mozambique also began integrating the planning and distribution of essential medicines and vaccines. Before each program managed its own commodities. There might be a day when antiretroviral drugs are delivered to a remote clinic and then, the next day, family planning commodities would be delivered. That inefficiency has now been eliminated. The government has also begun to partner with 67 private pharmacies to aid in the distribution of antiretroviral drugs.
Mozambique’s Ministry of Health is also improving its ability to track supplies as they move through the system by “leveraging technology investments that enable data visibility,” said Brito, “Data is vital to know where you need supplies. Matching supply with demand requires visibility.”
And visibility required linking every health facility in the country with a central information system. As recently as 2016, only 2% of Mozambique’s public health supply chain was online. The remaining 98% of the country’s 1,579 health facilities were offline and had to file paperwork that would be hand delivered to central warehouses to request supplies. Today, all public health facilities have the capacity to connect, at least once a week, to send and receive information about supply chain needs.
Mozambique’s COVID-19 vaccine campaign demonstrates the potential impact of these investments. The country has succeeded in vaccinating more than 96% of eligible adults. “I think that the fact that Mozambique maintained product availability during the pandemic and rolled out COVID-19 vaccines more quickly than other countries in the region is a testament to the investments made over the years in these supply chain improvements. It’s a great model for others to learn from,” said Emily Bancroft, President of VillageReach.
A variety of tools are available for health leaders seeking to measure and improve the performance of their public health supply chains. These include: the ASCM Global Health Supply Chain Maturity Model, the Logistics Systems Assessment Tool (LSAT), the Logistics Indicators Assessment Tool (LIAT), the National Supply Chain Assessment (NSCA) Toolkit, the Supply Chain Information System Assessment Maturity Model Assessment (SCISMM), and a Supply Chain Integration Framework which identifies often overlooked areas for investment to accelerate progress including: leveraging private sector capacity, professionalizing supply chain workforce, and ensuring that the supply chain reaches beyond health facilities to frontline health workers and volunteers in the community.
How can we help you?
believes that the quickest path to improving health outcomes to identify positive outliers in health and help leaders implement lessons in their own countries.
With our network of in-country and cross-country partners, we research countries that have made extraordinary progress in important health outcomes and share actionable lessons with public health decisionmakers.
Our research can support you to learn about a new issue, design a new policy, or implement a new program by providing context-specific recommendations rooted in Exemplar findings. Our decision-support offerings include courses, workshops, peer-to-peer collaboration support, tailored analyses, and sub-national research.
If you'd like to find out more about how we could help you, please click . Please consider so you never miss new insights from Exemplar countries. You can also follow us on Twitter and LinkedIn.
