Nepal: An exemplar in neonatal and maternal mortality reduction
Nepal has achieved exceptional reductions in maternal and neonatal mortality, by targeting vulnerable communities and expanding access to care.
CONTENTS
Introduction to Nepal
Nepal is a nation of 30 million people, located in South Asia, nestled between northeastern India and southwestern China. Health and social progress are enshrined in the country’s identity: Nepal’s commitment to improving health for all started in 1978 after the Declaration of Alma-Ata. This commitment was reaffirmed in 1990 at the commencement of Nepal’s multi-party democracy. The country underwent a series of political transitions over recent decades. In 2015, it ratified a new constitution that enshrines a right to health, mandating that the government provide basic and emergency health services for all citizens.
Through these transitions—and challenges such as a civil war and a destructive earthquake—civil society has helped keep the country’s health system progressing, promoting an emphasis on the importance of resilience. This progress is particularly impressive considering that Nepal faces unique geographical challenges inherent to being a highly mountainous country with many hard-to-reach communities.
The maps in Figure 1 reflect Nepal’s population density across three ecological zones in 2000 and 2020, as well as relevant administrative boundaries for the country. From 1982 until 2015, Nepal was divided into five development regions: Far-Western, Mid-Western, Western, Central, and Eastern. These regional boundaries have since been phased out. They were replaced by seven provinces in 2015: Sudurpashchim, Karnali, Lumbini, Gandaki, Bagmati, Madhesh, and Koshi. Figure 1 shows the current provincial boundaries and the former development regions, as well as the ecological zones that overlap within each administrative region.
Figure 1: Population density, ecological zones, and administrative boundaries in Nepal, 2000–2020

WorldPop (www.worldpop.org - School of Geography and Environmental Science, University of Southampton; Department of Geography and Geosciences, University of Louisville; Departement de Geographie, Universite de Namur) and Center for International Earth Science Information Network (CIESIN), Columbia University (2018). Global High Resolution Population Denominators Project - Funded by The Bill and Melinda Gates Foundation (OPP1134076). https://dx.doi.org/10.5258/SOTON/WP00675
Nepal’s gross domestic product per capita was US$1,337 in 2022, a large increase from US$224 in 2000. Our country selection analysis found that economic progress does not entirely explain Nepal’s progress in reducing neonatal and maternal mortality in recent decades. This narrative will highlight the key policies, programs, and interventions that contributed to rapid neonatal and maternal mortality reduction in Nepal. Nepal was also identified as an , , and vaccine delivery, where similar policies and programs played a role in the nation’s success. Additional details about Nepal are included in the section.
Key Insights
Removed user fees and introduced financial incentive programs
To improve access to care, Nepal removed user fees from delivery care services and provided cash incentives to women for accessing maternal and neonatal health services.

Nepal introduced a variety of financial assistance mechanisms to minimize barriers to accessing care. In 2005, the government introduced a geography-specific cash incentive to women to offset transport costs for institutional delivery. Nepal’s Safe Motherhood (Aama Surakshya) program was expanded in 2009 to remove user fees for delivery care in facilities nationally, including for C-sections. This policy introduced additional delivery-related incentives for health workers and hospitals and provided referral funds for emergency transfer. The government also introduced an incentive for women to complete four antenatal care visits. Since the introduction of these policies, Nepal has experienced substantial increases in ANC4+ coverage and institutional delivery rates.
Strengthened the network of female community health volunteers
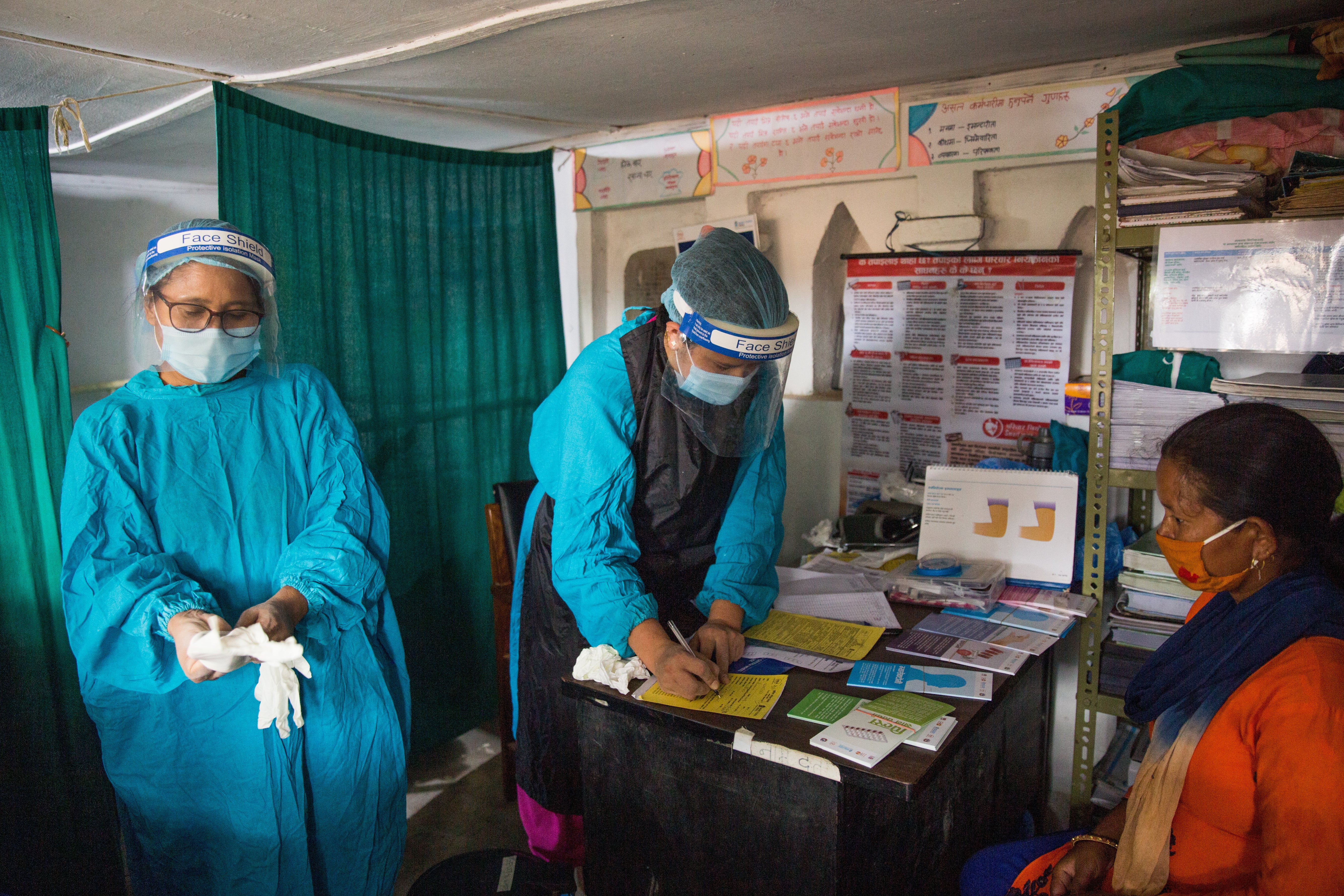
Nepal launched and expanded the scope of their ~51,000 female community health volunteers to extend the reach of the health system and better connect with communities.
Nepal’s female community health volunteers (FCHVs), introduced in 1988, are typically local women over 25 years of age who receive 18 days of training in various primary health care topics. FCHVs work at the community level, making door-to-door visits and providing services to clients in their homes to offer promotive and preventive health services. Starting with family planning, antenatal care, and immunization services, the FCHV program’s mandate expanded to include a variety of other maternal and child health services. FCHVs have been crucial in expanding healthcare access in Nepal, especially to rural and remote areas. By 2014, there were more than 51,000 FCHVs active in Nepal.

Scaled up safe abortion services to improve access
Nepal improved access to abortion by training a variety of healthcare professionals, increasing the number of facilities that could provide safe abortion services, and removing financial barriers.
Nepal legalized abortion in 2002, started training health professionals to deliver safe abortion services in 2004, and expanded the training to mid-level providers in 2008. As of 2021, the number of trained providers had tripled since 2009 to about 4,500. Nepal’s government also emphasized geographic accessibility of safe abortion services in rural areas. From 2011 to 2021, Nepal tripled the number of facilities that could provide safe abortion services, including some primary health care centers. The government also removed user fees from safe abortion services at public facilities. These strategies have helped improve access and mortality: nearly 80,000 women used safe abortion services annually in 2021, and abortion/miscarriage-related mortality decreased from 33% of overall MMR in 1990 to only 3% of overall MMR by 2019.
Contextualizing Nepal’s Progress in an Integrated Mortality Transition Framework (IMTF)
Nepal moved from phase II in 2000 to phase III in 2020 on the transition framework, demonstrating exemplary progress in improving maternal and neonatal health outcomes.
Progressing along the transition framework, Nepal experienced fertility declines and substantial expansions of health service coverage, aided by female community health workers, user fee removal, and financial incentives. Nepal’s maternal mortality ratio in 2020 was 174.4 maternal deaths per 100,000 live births, and its neonatal mortality rate in 2021 was 16.2 neonatal deaths per 1,000 live births Moving forward, Nepal will look to continue its trajectory into phase IV and beyond, prioritizing the closure of equity gaps in health service access and health outcomes.

Exemplars in Global Health program
The Exemplars in Global Health program aims to learn from countries that have made rapid progress in improving health outcomes and disseminate this evidence to inform health policy and funding decisions. Our aim is to research success stories from low- and middle-income countries and share findings that can be useful for leaders looking to act in comparable contexts.
In selecting Exemplar countries, we review evidence to identify countries that outperformed their peers in vital areas of public health, controlling for factors such as economic growth. In this way, we aim to provide more actionable, policy-relevant insight for stakeholders about how health progress can be made despite resource limitations.
Together with research partners and technical advisers, we conduct quantitative and qualitative analyses to validate our initial assessments and assess factors that contribute to a country’s exemplary performance.
Research in and across Exemplar countries could help ministries, nongovernmental organizations, and multinational bodies better deploy finite resources to address key public health issues in low- and middle-income countries.
By studying proven strategies to prevent disease, malnutrition, and other conditions that burden populations of low- and middle-income countries, we aim to create a list of data-driven narratives that can serve as resources for leaders looking to improve health within their own countries. The following narrative focuses on factors that contributed to rapid reductions in neonatal and maternal mortality in the Exemplar country of Nepal.
Nepal: An exemplar in neonatal and maternal mortality reduction

Ask an Expert
Our team and partners are available to answer questions that clarify our research, insights, methodology, and conclusions.
