Key Points
- Senegal’s highly successful comprehensive vaccination programs were among the main catalysts of its progress against U5M.
- Several of the nation’s most effective interventions came about through the Integrated Management of Childhood Illness (IMCI), both within communities and in facility-based care.
- At the community level, Senegal’s highly varied community health worker cadres were vital to the effective delivery of key interventions.
One important driver of Senegal’s success has been its comprehensive vaccination programs; this section begins with a brief examination of those programs, followed by other interventions that have been vital in reducing some of the most prolific causes of childhood mortality.
Vaccine Preventable Diseases
In 1992–1993, data from the Demographic and Health Surveys (DHS) showed that only 49 percent of Senegalese children ages 12 to 23 months had received all eight basic vaccine doses: the Bacillus Calmette-Guérin tuberculosis vaccine (BCG); three doses of diphtheria-pertussis-tetanus vaccine (DPT), measles vaccine, and three doses of polio vaccine.1
By 2000, Senegal’s immunization program provided these basic vaccines for children as well as yellow fever. In 2005, only 59 percent of the country’s children were receiving eight basic vaccine doses, as defined by DHS.1
By 2016, Senegal had introduced six additional vaccines to the national immunization program: hepatitis B vaccine, Haemophilus influenzae type b (Hib) vaccine, rubella vaccine, injectable polio vaccine (replacing oral polio vaccine), rotavirus vaccine, and pneumococcal conjugate vaccine (PCV).
Even with the increased logistical and administrative complexity of this expanded vaccination package, national coverage of the eight basic vaccine doses reached 70 percent by 2012 and has been maintained at or near this level.1 For DPT alone – considered the basic international benchmark for overall vaccine coverage – the vaccination rate rose from 51 percent in 1992 to 93 percent in 2017.2
The sections below outline Senegal’s path toward expanded coverage of the major vaccines in its national program.
Percentage of children aged 12-23 months with full and selected vaccinations
Measles
Measles vaccine was among the six included in Senegal’s Expanded Programme on Immunization in 1986.3 Initially introduced in a limited number of districts, it was scaled up nationally over the following year. Coverage was initially low (only 20 percent in 1986) but increased over time to cover more than half of all children (57 percent) by 1993.4
In 2001, Senegal implemented an eight-year strategic plan for eliminating measles. The following year, the government established a laboratory-based surveillance system for measles at the Ministry of Health (MOH) and the Institut Pasteur de Dakar.5
Building upon Senegal’s previously established polio-surveillance systems, the new program called for training community health workers (CHWs) to identify and monitor potential measles cases in their communities, and to report possible cases to a coordinating district nurse. For more on CHWs and their responsibilities, see the section on Community-Based Integrated Management of Childhood Illness.
The new surveillance program was an important sign of the national government’s seriousness about the measles campaign, and has proved to be a vital element in its success.
Measles mortality and vaccine coverage in Senegal
“Measles is one of the most monitored diseases in Senegal because there is routine surveillance with weekly notifications that are received every day,” said one interviewee. “As soon as there is a case, the notification circuit is very clear and people are trained on it, so that for measles we have a very efficient monitoring system that is currently implemented.”
While measles vaccination coverage has improved significantly since the turn of the century, it has more recently flattened out, edging up from 74 percent in 2005 to 82 percent by 2011 – and remaining at that level after the end of the study period in 2016.4 Interviewees reported that as of 2019, there had been no research on why coverage levels have remained so static.
In a frightening reminder of just how important achieving – and maintaining – minimum coverage levels can be, a 2009 lapse in measles funding led to an increase in cases, including an outbreak centered in Dakar, with continuous virus transmission from late 2009 to early 2010.5
In 2014, with support from Gavi, Senegal introduced a measles-rubella vaccine, adding the rubella vaccine to the second dose.6 Since then, transmission of measles has fluctuated – Senegal recorded 58 confirmed cases in 2015, and 159 in 2016.7
Meningitis
With funding support from Gavi, the MOH introduced the Haemophilus influenzae type b (Hib) vaccine into its immunization program in July 20058 as part of a pentavalent vaccine that protected against diphtheria, tetanus, pertussis, and hepatitis B.
Despite a comprehensive preparation phase that was supported financially and technically by Gavi, USAID, UNICEF, and the World Health Organization (WHO), the Hib immunization campaign faced some early setbacks. A 2006 evaluation found significant problems with the cold chain, with vaccines stored at temperatures outside the recommended temperature range of 2–8 degrees Celsius.8
Even with this early challenge, the program went on to show impressive gains. National Hib vaccine coverage among one-year-olds reached 89 percent in 2006 (one year after introduction), and 93 percent in 2016.9
National coverage for all three doses of pentavalent vaccine increased from 80 percent in 2010–2011 to 90 percent in 2016. However, an economic-equity gap remained, with 100 percent coverage for the wealthiest quintile, and 80 percent for the poorest.
These elevated rates of coverage translated into illness averted and lives saved. Hospitalization for Haemophilus influenzae meningitis in the Dakar region declined by 98 percent from 2002 to 2008. The national meningitis death rate decreased from 105 deaths per 100,000 children under five in 2000 to 37 in 2016 – a figure that included not only Hib-related meningitis, but meningococcal strains as well.10
Lower respiratory infections mortality and intervention coverage in Senegal
To jump-start progress against the meningococcal variant in the wake of a 1996–1997 meningitis epidemic that killed 25,000 people across sub-Saharan Africa, the Bill & Melinda Gates Foundation awarded a US$70 million seed grant to WHO and PATH in 2001 to establish the Meningitis Vaccine Project. The initial aim of this consortium was to develop a new vaccine against meningococcal meningitis in less than ten years.11
The result was MenAfriVac, officially introduced in 2010. The following year, Gavi approved Senegal’s plans to introduce this new meningococcal conjugate vaccine.12 In 2012, MenAfriVac was deployed in a preventive vaccination campaign throughout the highest-risk regions of Senegal. Since this campaign, the country has had no further outbreaks of meningococcal meningitis.
Pneumococcal Disease

Soon after Gavi was founded in 2000, the organization began supporting the introduction of PCV into the immunization programs of lower-income countries, including Senegal. In 2007, WHO recommended the adoption of PCV worldwide.13
However, there remained the question of which specific PCV type Senegal should use. In 2007 and 2008, a surveillance study sought to establish which type would be most suitable for Senegal’s epidemiological context.
This study, conducted at the Albert Royer Children’s Hospital in Dakar, measured nasopharyngeal pneumococcal carriage and pneumococcal infection in children under five, and identified the serotypes responsible for the majority of pneumococcal infections in this age group.
The study found a high rate of carriage and disease caused by Streptococcus pneumoniae serotypes targeted by the PCV13 vaccine type, with the PCV10 and PCV7 vaccines achieving lower levels of coverage against Senegal’s predominant pneumococcal strains.13
Due to a shortage of PCV13 – and the discovery that Senegal’s cold chain was not yet ready to support the introduction of the vaccine – the rollout was delayed from an initial start date of 2012 until 2013, when Senegal became the 34th out of 73 Gavi-eligible countries to introduce PCV13 into its routine immunization program.14 15
Gavi provided about 80 percent of the funding for the PCV13 rollout, with WHO, UNICEF, and the Senegalese government providing the rest. While Senegal anticipated that its PCV co-financing contribution would increase to 35 percent by 2016, rising exchange rates prevented this from happening by the end of the study period.16
Rotavirus
In 2009, WHO recommended worldwide introduction of the rotavirus vaccine against childhood diarrhea. Between 2011 and 2015, Gavi funded the vaccine in several African countries, including Senegal.17
In preparation for a 2014 rollout, Senegal began acting upon WHO’s recommendations for the introduction of new vaccines, including planning and budgeting, conducting needs assessments, and evaluating cold chains and supply chains.18 This work was done with funding support from Gavi, and technical support from both Gavi and the New Vaccines Technical Working Group.
Senegal’s deployment of the rotavirus vaccine was delayed because the government opted to proceed first with PCV, which Gavi had recommended for introduction at about the same time. This ranking of priorities was largely based on disease burden data and the country’s capacity to support each of the two rollouts. See section on pneumococcal above.
PCV was therefore introduced in 2013, with rotavirus debuting in November 2014.16 Gavi continues to provide substantial support for the rotavirus vaccine program, originally accounting for about 80 percent of funding, with WHO, UNICEF, and the government providing the remaining 20 percent. By the end of the study period in 2016, Senegal’s contribution to the co-financing agreement had increased to 26 percent.
The PCV and rotavirus vaccine campaigns shared some important commonalities. In both cases, practitioner education started with central-level instructions for regional and district managers, who then cascaded the one-day trainings to frontline health workers. Each district was allocated one week to complete trainings for all health facility staff within the district. Following the trainings, district managers conducted supervisory visits to monitor the initial introduction of the vaccines.
Diarrhea disease mortality and intervention coverage in Senegal
Both campaigns also benefited from improvements to cold chain and supply chain management, though Senegal’s overall performance on these fronts has been mixed.
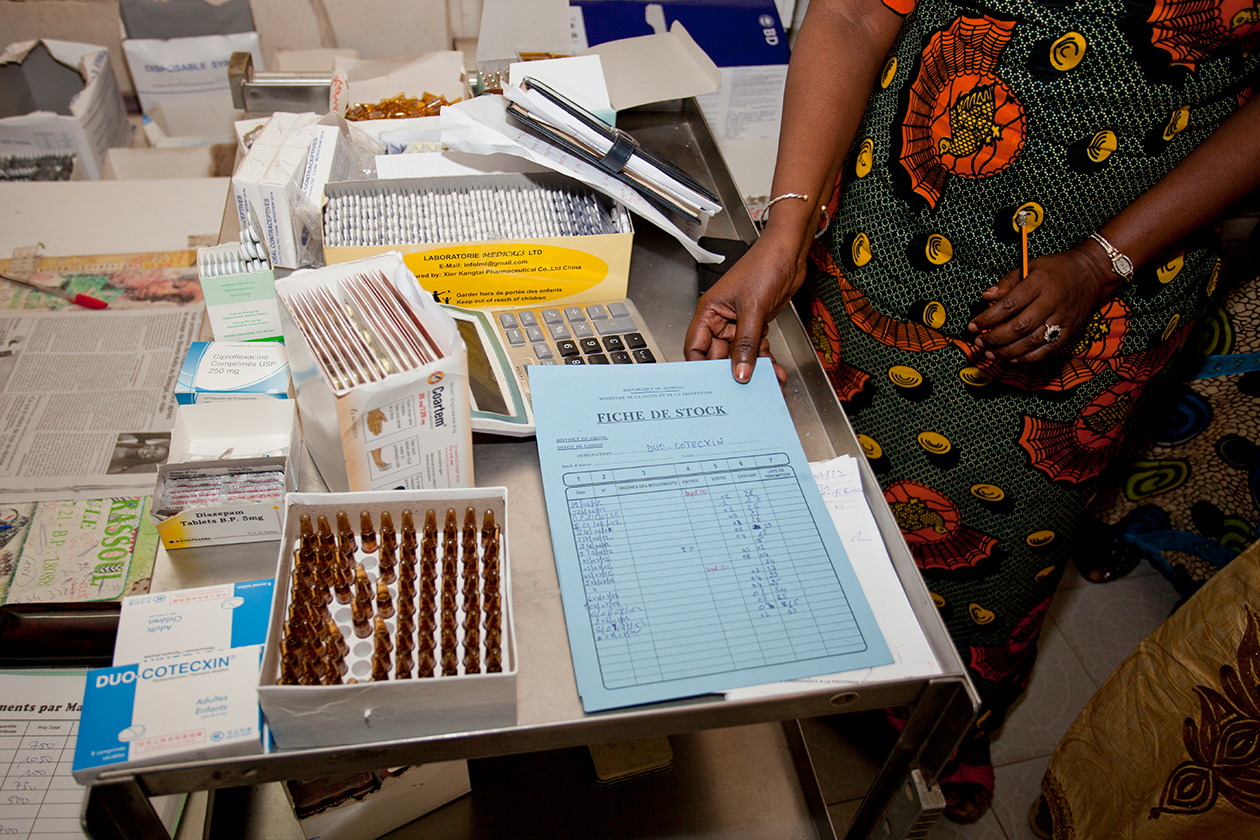
An evaluation of the PCV rollout identified concerns about cold chain storage capacity and temperature regulation.16 However, a 2015 evaluation of the country’s medical supply chains found several positive developments, including an updated essential medicines list, a network of health workers trained in supply chain management, and procurements of necessary vehicles to improve distribution of essential commodities.20
In the end, according to interviewees, cold chain management had a limited effect on the quality of vaccine delivery, due to the widespread use of vaccine vial monitors that helped delivery personnel identify whether a given supply was still usable.
Tetanus
In 1999, the Maternal and Neonatal Tetanus Elimination (MNTE) Initiative was launched by UNICEF, WHO, and United Nations Population Fund (UNFPA). The aim of MNTE was to reduce cases of neonatal tetanus to less than one case per 1,000 live births throughout all countries that had not already achieved the standard for elimination at the time of launching. Senegal was one of those countries.
In preparation for launching MNTE, Senegal underwent a review of subnational maternal and neonatal tetanus case data, supplemented by field visits, to identify high-risk districts for maternal and neonatal tetanus – a category that came to include less than 20 percent of the country.21
The national government, supported by WHO and UNICEF,22 developed a plan to provide vaccines and supplies yearly, to ensure they were consistently available at central and regional levels.
Senegal launched campaigns in the high-risk areas, calling for three properly spaced doses of tetanus toxoid vaccine to all women of reproductive age.21
Vaccine supply levels were adjusted during the course of implementation, to account for consumption rates. As a result, tetanus vaccination coverage improved. The percentage of women receiving at least two doses of tetanus toxoid was 45 percent in 2000, 67 percent in 2005, and 84 percent in 2015.
Tetanus protection at birth increased from 62 percent in 2000 to 69 percent in 2010 and 82 percent in 2016.23 All districts in Senegal reached their goal of less than one case of neonatal tetanus per 1,000 live births by 2009.22 The number of newborns dying from tetanus decreased from 770 deaths per 100,000 live births in 2000 to 74 in 2016.10
Overall, across all vaccines, a statistical analysis from the Institute for Health Metrics and Evaluation (IHME) found that 30.7 percent of the reduction in under-five deaths was attributable to vaccine interventions.73
Integrated Management of Childhood Illness
A large share of Senegal’s non-neonatal under-five mortality is attributable to three disease categories: diarrheal illnesses, respiratory infections (especially pneumonia), and malaria. In 2000, these three conditions together accounted for 44 percent of all deaths among Senegalese children under five, and 31 percent in 2015.
The country’s impressive progress against this lethal trio is due in no small part to its successful implementation of a holistic prevention and treatment protocol known as Integrated Management of Childhood Illness (IMCI).
Developed by WHO and UNICEF in 1995 as a comprehensive approach to improving child health systems in low-income countries, IMCI seeks to strengthen both health facilities and community-based health practices.24
IMCI focuses on improving health care providers’ abilities to diagnose and treat the most common childhood illnesses in countries suffering from high rates of under-five mortality, including through the assessment and improvement of family and community health behaviors.25
This section looks at Senegal’s experience with IMCI, both at the health facility level and at the community level.
Facility-Based Integrated Management of Childhood Illness
In 1996, Senegal’s national government requested meetings with WHO officials to discuss the potential introduction of the IMCI strategy, which was novel at the time. WHO organized several presentations on IMCI that included the experiences of countries that had already begun using it, such as Uganda.
As a result of these meetings, Senegal decided to adopt IMCI as its core strategy for reducing child mortality. An initial pilot of facility-based IMCI (FB-IMCI) began in 1999 in Darou Mousty, a compact district in the country’s northwest.
The pilot revealed some early flaws – despite receiving IMCI training using WHO guidelines, only 16 percent of nurses in the pilot had followed FB-IMCI diagnostic and therapeutic procedures.
The Darou Mousty pilot influenced the later national rollout of FB-IMCI. It showed that basic training and in-service courses should place greater emphasis on FB-IMCI procedures, and it highlighted the need for regular supervision to achieve better outcomes.25
One interviewee said, “The question of supervision remains a constraint of the system today, but [as a result of the study] the post-training follow-up and the supervision of providers were reinforced as key elements of implementation of the IMCI strategy.”
In 2000, the FB-IMCI pilot expanded to three additional districts (Kaffrine, Kebemer, and Sedhiou), chosen because of their relatively high under-five mortality rates and challenging geographic locations. The results were promising, especially with regard to increased engagement of mothers on issues pertaining to their children’s health. Inclusion of caregivers in decisions regarding their children’s care was one of the aims of the IMCI strategy.
A 2001 evaluation of the second FB-IMCI pilot program found high levels of readiness and quality. For example, 96 percent of malaria cases in the FB-IMCI locations received appropriate antimalarial treatments, compared with 70 percent in non-IMCI facilities.
FB-IMCI protocols also appeared to sharply decrease the overuse of antibiotics – 80 percent of children without pneumonia at non-IMCI facilities had received unnecessary antibiotics, whereas the rate at IMCI locations was only 30 percent.26
Furthermore, the evaluation found strong evidence that FB-IMCI reduced systemic health costs. Expenses for treatment of respiratory infections were 563 percent higher at facilities that were not using FB-IMCI, compared with those that were. Diarrhea treatment costs were 302 percent higher. These striking differentials were mainly due to overuse of antibiotics and cold medicines at non-IMCI facilities.26
Such assistance was crucial to the national rollout. As one interviewee explained, “It’s thanks to the conjunction of all [donors and partners] that IMCI experienced a very large scale.” A final scale-up took place beginning in 2013 to build upon these earlier gains.
Nurses were trained on the FB-IMCI protocols for 11 days and supervised for a brief period thereafter by district health teams, who themselves had been trained by central-level teams. According to interviewees, this IMCI-focused supervision ensured better coordination of previously separate programs focusing on diarrhea, malaria, and pneumonia.
One major challenge was staff attrition among nurses, who would be the main providers of FB-IMCI. The MOH recognized this problem relatively early, and in 2002 began introducing ways to incorporate FB-IMCI training into the preservice training curriculum for nurses.
In response, Senegal adopted the combination of sulfadoxine-pyrimethamine and amodiaquine for malaria treatment. Three years later, acting on new WHO recommendations, Senegal introduced artemisinin-based combination therapy (ACT).27 By 2014, ACT was offered at all health facilities across the country.28
In the meantime, Senegal introduced another strategy to reduce malaria. In 2007, the MOH identified the high cost of treating malaria without confirmatory evaluation, and introduced rapid diagnostic tests (RDTs) in advance of beginning treatment – three years ahead of WHO’s recommendation of such testing.
Senegal’s interest in RDTs derived in part from its recent experience with chloroquine resistance; the MOH wanted to prevent ACT from falling into a similar obsolescence.
“Apart from ACTs, we had nothing else. They were the most effective medicine and there was nothing behind them,” explained one interviewee. “Which meant that if the ACTs did not work anymore, we would have problems. By misusing the medicine, we risked the phenomenon of resistance. So it was better to make the effort to test, to treat real cases and use the medicine efficiently.”
For more details on Senegal’s campaign against malaria, see the section on Additional Interventions to Reduce Malaria.
Community-Based Integrated Management of Childhood Illness
A community-level introduction of IMCI would be crucial to Senegal’s campaign to reduce under-five mortality, due to the high levels of need in the country’s rural areas. The government sought to extend case management of childhood illness more comprehensively from health facilities to towns and villages.
The plan was to build community-based IMCI (CB-IMCI) upon the existing community-based government malaria program to address diarrhea and acute respiratory infections (ARIs) such as pneumonia. For example, oral rehydration therapy (ORT) was added to IMCI in 1996.
Community Health Worker Programs
The heart of Senegal’s community health system has long been its diverse cohort of CHWs, who are directly linked to the country’s health systems at several levels.
This community health system is especially critical in a country suffering from a chronic shortage of doctors and nurses. The WHO guideline is that countries should have 4.45 doctors, nurses, and midwives for every 1,000 people .72 For every 1,000 Senegalese, however, there is less than half a health worker (0.377), and the shortfall is even more acute outside of Dakar and other urban areas.29

Five main CHW groups address a wide range of health priorities. Two of the most prominent cadres are the matrones and agents de santé communautaire (ASCs). These two groups overlap significantly, with many matrones also serving as ASCs, and vice versa.30 What distinguishes these two CHW groups is their work in Senegal’s cases de santé, or health huts, which have been the backbone of Senegal’s community health system since the 1950s, providing basic treatment for common diseases.31
In 2006, Senegal adapted its guidelines for treating childhood diseases to reflect the new CB-IMCI program. To maximize the odds of success, the government adopted both health hut and home-based delivery approaches. In 2013–2014, there were approximately 2,300 health huts and more than 16,000 health care providers and advocates within the community health system.30
Within the health huts, matrones focus on maternal and newborn health, acting as skilled birth attendants. ASCs provide basic health care at the huts and in the broader community, including such services as wound dressing, disinfection, antidiarrheal care, treatment of malaria and respiratory diseases, and provision of contraceptives.
The USAID-supported bajenou gokh program has provided such vital services as antenatal and postnatal visits, child immunization, family planning consultations, and campaigns against gender-based violence.
A fourth CHW cadre is the relais communautaires (relais). Like the bajenou gokhs, the relais focus on health promotion and education, but they also cover a broader range of under-five mortality issues.
Finally, the dispensateurs de santé à domicile extend the reach of the community health system from the health huts into the home. While they have traditionally focused on malaria, CB-IMCI has broadened their portfolio to include diarrhea and pneumonia treatment as well.
The preparation of CHWs for the increased responsibilities of CB-IMCI relied on a training-of-trainers approach. Health post nurses who had received instruction in FB-IMCI conducted five-day sessions for local community health workers,33 with the nurses required to provide ongoing monthly supervision to the CHWs. As a reinforcement of this basic training, supervisors conducted follow-up visits.
The decision to expand the role of CHWs under CB-IMCI was not met with universal approval. One cause of concern was the CHWs’ ability to properly administer antibiotics. In response, the government’s 2003–2004 preparations for CB-IMCI included an advocacy campaign aimed at health care professionals, explaining the merits of allowing trained CHWs to use antibiotics in treating pneumonia.
In the years since the introduction of CB-IMCI, studies have presented a generally positive picture of CHW performance. A 2007 review found that 90 percent of Acute Respiratory Infection (ARI) cases managed by CHWs were correctly classified, soundly managed, and followed through to completion.34
Community-based health interventions were also making headway against another major cause of under-five mortality – diarrhea. In 2009, the CB-IMCI program added zinc supplementation to its portfolio, and by the following year more than 1,600 health huts provided oral-rehydration treatment (ORT), across more than three-quarters of Senegal’s health districts.
Senegal sought to build upon these achievements. By 2014, the first community health strategic plan was developed, followed by the establishment of a community health unit at the MOH.
Yet even with this increased formalization of the national government’s role, towns and villages still had substantial influence over their own health affairs.
While the government must approve the creation of new health huts, the community health system otherwise operates with a high degree of local autonomy.
A survey from 2014 found that the CB-IMCI program in Senegal was the most cost-efficient per capita out of seven sub-Saharan countries reviewed. This study also found that Senegal’s CHW attrition rates were impressively low (5 percent)35 – an outcome that was probably attributable not only to the CHWs’ dedication, but also because they received payments for handling their newly expanded duties under CB-IMCI.
Although Senegal began implementing payment plans as early as 2012, interviewees noted that as of 2019 the compensation still did not cover all CHWs’ work under CB-IMCI; however, each CHW did receive compensation of 2,500 CFA per week (about US$4.30) for their work in the malaria program.
Additional Interventions to Reduce Malaria
In 2013, incidence of malaria varied widely in Senegal, with the highest transmission rates (25 or more cases per 1,000 people) occurring in the south and southeast. The northern region had the lowest rates (5 or fewer), with moderate transmission across a central band spreading eastward from Dakar (5 to 25).36
Malaria incidence per 1000 population in Senegal, 2013

In addition to CB-IMCI and FB-IMCI programs, Senegal relied upon several stand-alone malaria prevention strategies, notably indoor residual spraying, intermittent preventive treatment, and insecticide-treated nets (ITNs). These interventions are discussed below.
Insecticide-Treated Nets
In response to WHO recommendations, the Senegalese government introduced a campaign in 1998 to sell ITNs at a reduced cost through subsidy agreements between private-sector net distributors and facility health committees – and with significant support from USAID and the Global Fund.37
ITNs had been used previously in Senegal, but on a limited basis through small-scale, donor-supported initiatives. In 2007, Senegal began issuing ITNs free of charge – a policy that reflected both WHO recommendations and the fact that the President’s Malaria Initiative (PMI) had just chosen Senegal as a funding recipient.38
The campaign provided nets to all households, with a target of placing ITNs in each sleeping space, or at least one for every two individuals in a household. Senegal decided to conduct mass campaigns every two years, based on local research suggesting that this was the nets’ useful life span (a duration that fell short of the three years recommended by WHO).28
Noting the particular risk of malaria to children under five, the MOH began a national campaign aimed specifically at this age group in 2009. By early 2013, 6.9 million long-lasting insecticide-treated nets (LLINs) had been distributed across the country, reaching all districts. Between July 2013 and November 2014, Senegal distributed an additional 3.9 million nets to further ensure universal coverage.37
In 2012, to complement its population-wide mass distributions, Senegal began a PMI-funded facility-based distribution effort to ensure that all pregnant women received nets in the course of their antenatal care.
In addition, Senegal undertook a public engagement strategy known as ABCD (Atteindre les Bénéficiaires de la Communauté à travers les Districts), incorporating door-to-door and community-wide outreach activities.
As a result of these and other initiatives, ITN coverage rates increased from 20 percent of all households in 2005 to 63 percent in 2010 and 82 percent by 2016. The proportion of children under the age of five sleeping under an ITN increased from 7 percent in 2005 to 35 percent in 2010 and 67 percent in 2016.39
Malaria mortality and intervention coverage in Senegal
Intermittent Preventive Treatment
Intermittent preventive treatment (IPT) involves multiple administrations of antimalarial medicine throughout a peak malaria season, in order to sustain drug concentrations in the blood throughout the period of greatest risk.
In 2000, the African Summit on Roll Back Malaria in Abuja, Nigeria, recommended that at least 60 percent of pregnant women be covered by antenatal malaria interventions (including IPT) by 2005. Senegal was one of the countries that committed to this target. It began offering IPT for pregnant women two years ahead of the deadline, providing them with sulfadoxine-pyrimethamine treatments at antenatal care sessions.40
In 2005 a study led by the parasitology laboratory at Cheikh Anta Diop University in Dakar found that giving chemo-prophylactic malaria treatment (one dose of sulfadoxine-pyrimethamine and one dose of artesunate) to children under five reduced the incidence of malaria by 86 percent.41
In response to this striking result, the National Malaria Control Program designed an IPT for children regimen, with support from the Global Fund and district health teams. A 2006–2007 pilot in Tivouane District showed that IPT for children could be delivered effectively at larger scale.
In 2008, Senegal undertook a three-year implementation pilot in the districts of Mbour, Bambey, and Fatik, and introduced a seasonal IPT administration for children between the ages of three months and ten years.42 By 2010, IPT was offered to children in 46 rural and semi-urban areas.
In 2012, WHO issued a recommendation for IPTc – now known as seasonal malaria chemoprevention (SMC)42 – for those parts of the Sahel that experience highly seasonal patterns of malaria transmission.43 The Senegal pilot helped inform the WHO policy recommendation for this region.44
The IPT program has encountered some challenges. A study of the initial implementation between 2008 and 2010 found that CHWs were administering excess sulfadoxine-pyrimethamine to mothers, failing to routinely check for side effects, and often giving the treatment to children above the age of ten. As a result of these findings, health workers underwent training to reinforce treatment guidelines.42
Indoor Residual Spraying
In 2007, Senegal introduced indoor residual spraying in a single northern district (Richard Toll), then scaled up its pilot program in 2010 to six districts45 (Nioro, Vélingara, Guinguinéo, Koumpentoum, and Malem Hodar, in addition to Richard Toll), which the National Malaria Control Program had chosen because they experienced high levels of transmission during rainy peak malaria seasons.
Senegal switched from pyrethroid-based insecticides to non-pyrethroids in 2015, due to heightened resistance to deltamethrin among anopheline mosquito populations.37 Also that year, the country’s indoor residual spraying strategy shifted from blanket spraying to focal spraying – in other words, spraying only within districts where malaria incidence was at least 30 cases per 1,000 people.
This adaptation was intended as a more cost-effective approach than blanket spraying, but after a yearlong trial in four districts, focal spraying was found to be the slightly more expensive strategy.37
Indoor residual spraying coverage levels during the study period have been uneven, increasing from 3 percent in 2006 to 12 percent in 2012–2013, then down to 9 percent in 2014 and only 5 percent by 2016, as implementation shifted to focal spraying.46 47
In response to 2016 data showing a decline in malaria despite the uneven coverage of indoor residual spraying, government officials began discussions about discontinuing indoor residual spraying due to its low cost-effectiveness in moderate-endemicity, low-mortality settings compared with ITNs and other preventive tactics.
A statistical analysis from the Institute for Health Metrics and Evaluation (IHME) found that 5.2 percent of the reduction in under-five deaths was attributable to insecticide-treated nets and indoor residual spraying.73
Malnutrition
While Senegal – a country with limited arable land – has long implemented nutrition programs of various kinds, these efforts gained momentum after the 1994 currency devaluation, which spurred Senegal’s government to seek ways to combat the spreading malnutrition that had resulted from a spike in food prices. (For a more detailed treatment of the country’s nutrition and antistunting policies, see the Exemplars in Global Health report on Stunting in Senegal.)
One major post-devaluation nutrition measure was the Projet de Nutrition Communautaire / Community Nutrition Project (PNC), which ran through 2000. It advanced a variety of community-based nutrition programs, including child growth monitoring, behavior change communication, and efforts to enhance food security.
In 2000, Abdoulaye Wade was elected president of Senegal, and along with his wife, he made nutrition a priority. In 2001, Wade gave nutrition its own line in the national budget for the first time. He also focused the country’s nutrition efforts into a main operating body, the Cellule de Lutte Contre la Malnutrition (CLM), which has served as the driver of nutrition programming ever since.
In 2002, the CLM and the World Bank launched the Programme de Renforcement de la Nutrition (PRN), which built on the foundations laid by the PNC. The new program was designed in a series of workshops that included members from all nutrition-related industries, the Ministry of Finance, donors, and nongovernmental organizations.
The inclusiveness helped ensure that the PRN would draw upon a large reservoir of global evidence and technical expertise. It also generated buy-in from numerous ministries, as did the fact that those ministries received incentives to provide training, equipment, and technical support.
Such multisector cooperation is widely credited with Senegal’s successes in addressing malnutrition. “Here in Senegal, this multisectoral approach is an asset for us. It enables different stakeholders to work together to identify interventions, find synergies and complementarities,” one interviewee explained. “That's an important aspect, and I don’t think that there are as many countries worldwide that have achieved such a feat.”
The PRN began screening for acute malnutrition among children under five, identifying malnourished children, and providing support and treatment within the community setting. This adaptation began with a pilot in Kolda – a predominantly rural southern region with high rates of acute malnutrition – and later spread to other areas.
The program also established recovery and nutritional rehabilitation centers to treat severely malnourished children who required in-patient care (usually lasting approximately ten days), and to teach local mothers how to prepare nutritious meals.
This adaptation to the PRN called upon relais to identify malnourished children and treat them at the community level, while severely malnourished children were referred to the recovery and nutritional rehabilitation centers.
Nutritional deficiencies mortality, child growth and intervention coverage in Senegal
Overall, the PRN improved on the reach of the PNC. It expanded the initial coverage of the PNC from 14 local (mainly urban and peri-urban) communities to 385 communities across all regions of Senegal.
According to interviewees, the availability of funding was also a major factor in the growth and relative success of the PRN. Senegal annually committed to increasing funds to the CLM for the implementation of the program, with approximately 200 million CFA francs of direct funding to nutrition allocated in 2002 – a figure that had increased to 3 billion CFA francs by 2017.
Neonatal Interventions
Senegal’s neonatal mortality rate dropped by 38 percent during the study period, from 35 deaths per 1,000 live births in 2000 to 22 in 2016.48
This decline in neonatal mortality lagged behind the country’s decline in overall under-five mortality, which is typical even among other exemplar countries. However, Senegal’s progress in reducing neonatal mortality was admirably broad – with declines across all wealth quintiles, and some narrowing of the outcome gaps between high-income and low-income categories.49
These improvements were the result of interventions during both the antenatal and neonatal stages. In this section of the report, we discuss each of these stages in turn.
Antenatal Care
During the 2000–2016 study period, Senegal’s efforts to improve attendance at all four antenatal care (ANC) visits were mainly indirect, leveraging broader interventions aimed at strengthening the community health system in general.
In 1992, 75 percent of mothers attended at least one ANC visit. The minimum number of visits prescribed by WHO, however, was not one, but four – and only 13 percent of expectant mothers attended all visits.
Neonatal disorders mortality and intervention coverage in Senegal
Senegal sought to strengthen ANC through its varied and extensive CHW program, relying heavily on one cadre in particular – the bajenou gokhs.
These volunteers were well-positioned to improve ANC outcomes in their communities. Senegal has a deep culture of respect for older women, and this prestige was a powerful lever for promoting sound health practices, including early pregnancy detection, encouragement and facilitation of ANC visits, and dissuasion of social norms that act as barriers to accessing ANC, such as the concealment pregnancies.50
To carry out these varied and sensitive tasks, bajenou gokhs attended training sessions lasting two or three days, and received supervisory visits from MOH personnel, sometimes accompanied by representatives from USAID and other partners.
As compensation, bajenou gokhs received some job-related benefits, such as the use of mobile phones during community health campaigns, and per diem payments and transportation reimbursement to cover expenses related to training activities.
Bajenou gokhs carried out their work in collaboration with relais, and in 2014 were integrated into village committees – typically consisting of village chiefs, women's groups, youth associations, religious leaders, and ACSs.
These committees played a watch-and-warning role in the public health affairs of the community. They provided notifications of neonatal and maternal deaths, and resolved local cases of missed vaccinations and antenatal sessions.
While the bajenou gokhs have been instrumental to improving ANC access, there are not enough of them to go around. In 2014, there were 3,406 bajenou gokhs, well under the 12,000 required to reach the target of 1 per 100 households.30
Their work remains as important as ever. While the proportion of expectant mothers attending four or more ANC sessions recommended by WHO has risen impressively – to 40 percent in 2005 and 53 percent in 2016 – there is ample room for improvement.51
In addition to community-level programs encouraging antenatal care visits and other basic interventions, another vital component of Senegal’s ANC campaign was prevention of mother-to-child transmission of HIV (PMTCT).
In 2004, Senegal introduced its protocol for PMTCT, which involved oral treatment (with zidovudine) for the mother starting at 34 to 36 weeks into a pregnancy, and every three hours during childbirth (or intravenously where necessary). Subsequent to delivery, the newborn received treatment for one week.
The program began in Dakar due to the higher prevalence of HIV in the city, and by 2006 PMTCT programs were available in 11 of Senegal’s 14 regions.52 In 2010, PMTCT coverage was 23 percent, increasing to 57 percent by 2016.53
In 2012, Senegal adopted WHO’s B+ protocol, which entailed lifelong administration of a three-drug combination for HIV-positive pregnant women, with breastfeeding and antiretroviral prophylaxis for their infants.54
The percentage of HIV-positive pregnant women receiving antiretroviral therapy increased from 23 percent in 2010 to 48 percent in 2013 and 57 percent in 2016. The number of HIV-exposed children who remained uninfected also improved, from 15,000 in 2003 to 30,000 in 2016.55
There is still much ground to cover. While the percentage of women aware of PMTCT rose during the early phase of the program – from 22 percent in 2005 to 37 percent in 2010 – it declined to 28 percent by 2016. In addition, rates of early infant diagnosis remained low, nudging up from 9 percent in 2008 to only 13 percent in 2016.55 55
Senegal has also sought to improve antenatal care by offering iron and folic acid supplementation to pregnant women, a policy that has been in place for several decades.56
The percentage of women in Senegal who received iron tablets or syrup at ANC sessions was 91 percent in 2005 and 95 percent in 2016.57 Data from the Demographic and Health Survey and Service Provision Assessment show that 84 percent of health facilities stocked iron or folic acid in 2016.58 According to a 2016 DHS review of 849 observed antenatal care visits, health care providers gave or prescribed iron and folic acid tablets in 87 percent of cases.27
Several pilot projects have also tested delivery of iron and folic acid supplements through CHWs, and found them to be successful in increasing compliance.59 Randomized control trials have indicated that giving supplements for free during ANC visits is more effective than issuing prescriptions.60 Yet despite these trials, free iron and folic acid are not yet available across the country.
Neonatal Resuscitation and Care
Before 2006, basic equipment for neonatal resuscitation in Senegal was regularly available only at regional hospitals and sometimes at health centers, but not at smaller health posts.34
That year, in an effort to reduce neonatal mortality due to asphyxia, the MOH decided to equip health centers and health posts alike with training and “neonatal corners” that contain essential equipment for the treatment of newborns.
According to the UN Commission on Life-Saving Commodities, that equipment includes at minimum a neonatal mask and bag, a suction device, and a training mannequin.61 Interviewees reported that by 2019, neonatal corners had been established across the country.
This equipment, although helpful, could not comprehensively address challenges in neonatal care. In approximately half of facilities surveyed in one study, this essential gear simply went unused – mainly because of health worker turnover and the districts’ failure to train new providers in the use of the equipment.34
In an effort to train more health care workers in neonatal resuscitation, the MOH coordinated a USAID-supported national plan to begin implementing the Helping Babies Breathe curriculum by 2013.62
The Helping Babies Breathe Global Development Alliance was established in 2010 by five core partners (American Academy of Pediatrics, USAID, Laerdal Global Health, Save the Children, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development) to provide training for basic neonatal resuscitation in resource-limited settings. However, interviewees said the Helping Babies Breathe initiative suffers from a lack of coaching capacity, an absence of standards for neonatology units, and gaps in monitoring and evaluation.
It was clear that Senegal needed to improve access to advanced health facilities. Rates of facility-based delivery in Senegal were below the halfway mark throughout the 1990s, hovering at 47 percent in 1992 and 49 percent in 1999, held down by low rates in rural areas (30 percent in 1992 and 32 percent in 1999).
In the new century, the geographic disparity began to narrow, with rural rates of facility-based delivery rising to 47 percent in 2005 (compared with an urban rate of 89 percent). Economic gaps were also closing, albeit gradually. The facility-based delivery rate for the lowest wealth quintile in Senegal was 30 percent in 2005 – better than 24 percent in 1997, but still far lower than 94 percent for the highest wealth quintile.49
This policy applied only to public health centers, excluding private and traditional facilities. To compensate providers, the government gave them US$50 for simple cesareans and US$70 for complicated cesareans,64 and subsidized kits of basic delivery supplies.
The FDCP was initially piloted in the five poorest regions of the country (Kolda, Ziguinchor, Tambacounda, Matam, and Fatick) to identify the feasibility of the policy among the lower wealth quintiles.65 This was an example of a standard Senegalese practice of selecting high-risk areas for the piloting and rollout of interventions in an effort to reduce geographic and economic health inequalities.
A 2006 evaluation of the pilot found that facility deliveries at the health post and health center levels rose by 77 percent between 2004 and 2006 for FDCP regions, while the increase was only 19 percent for non-FDCP regions. The policy also led to a 49 percent increase in referrals from health posts within a single year.66
In January 2006, the FDCP was extended to the remaining regions in Senegal, except Dakar. The program expanded into the capital city in 2012.
National survey data confirms that the proportion of mothers who delivered in health facilities was rising. In 1997, 78 percent of mothers in urban areas were already delivering in a facility – a proportion that rose to 92 percent by 2015. During the same period, facility-based deliveries in rural areas almost doubled, from 33 percent in 1997 to 65 percent in 2015.67
The data suggests not only that mothers and babies benefited directly from high-quality care at crucial moments in the delivery process, but also that they were in closer contact with the health system throughout the critical first 1,000 days. As a result, they were more likely to receive messages about important behaviors like breastfeeding and proper nutrition. Indeed, the national rate of exclusive breastfeeding improved from 11 percent in 1997 to 36 percent in 2016.68
Another important improvement in neonatal care was the active promotion of skin-on-skin contact between newborns and their mothers – a practice known as kangaroo mother care (KMC).
A retrospective study conducted at Albert Royer Children’s Hospital in Dakar from July 2011 to July 2013 found KMC for low birth weight infants to be “highly effective in our context,” with a recommendation for national scale-up.69
In November 2013, 116 health workers had received KMC training at 22 health centers and 7 hospitals, with a long-term plan to introduce KMC to around 1,000 health centers across the country.70
In an effort to close the persistent gap between the neonatal mortality rate and the broader under-five mortality rate, Senegal adapted its IMCI program in 2016 to include neonatal care protocols.71 This adaptation was led by an MOH working group and facilitated by the integration of the neonatal and maternal health departments into a single unit.
Decomposition
A decomposition analysis undertaken in collaboration with the Institute for Health Metrics and Evaluation (IHME) at the University of Washington identified the top interventions and risk factors that contributed to reductions in under-five deaths in Senegal. These interventions and risk factors can be seen in the bottom two bars of the visualization below.
- Some of the largest contributors to reduction in under-five mortality were health system interventions, which were responsible for 58 percent of the reduction in under-five deaths from 2000 to 2017.
- Within this, vaccines (especially Hib vaccine, PCV, and rotavirus vaccine) were a significant factor, and were attributed to 30.7 percent of the reduction.
- Beyond health system interventions, reductions in other communicable disease risk factors, population age structure, and reduction in child growth failure were also found to have significant contributions to reduction in under-five deaths.73
Decomposition analysis
-
1
Received all 8 basic vaccinations [Senegal]. STATcompiler. Rockville, MD: The DHS Program. https://www.statcompiler.com/en/. Accessed Jan 23, 2018.
-
2
Monitoring and Surveillance. World Health Organization website. https://www.who.int/immunization/monitoring_surveillance/en/. Published July 15, 2018. Accessed April 24, 2019.
-
3
Mbengue, Sarr M, Faye A, et al. Determinants of complete immunization among Senegalese children aged 12–23 months: evidence from the demographic and health survey. BMC Public Health. 2017;17:630.
-
4
Measles vaccination received [Senegal]. STATcompiler. Rockville, MD: The DHS Program. https://www.statcompiler.com/en/. Accessed August 24, 2018.
-
5
Dia N, Fall A, Ka R, et al. Epidemiology and genetic characterization of measles strains in Senegal, 2004-2013. PLoS One. 2015;10(5):e0121704. https://doi.org/10.1371/journal.pone.0121704. Accessed July 3, 2019.
-
6
Senegal introduces pneumococcal, measles-rubella vaccines. Healio, Infectious Disease News. November 12, 2013. https://www.healio.com/infectious-disease/vaccine-preventable-diseases/news/online/%7B66eb4805-1b66-4c17-8902-576ee36a91cd%7D/senegal-introduces-pneumococcal-measles-rubella-vaccines. Accessed December 28, 2018.
-
7
Masresha BG, Dixon MG, Kriss JL, et al. Progress Toward Measles Elimination — African Region, 2013–2016. MMWR Morb Mortal Wkly Rep. 2017;66:436–443. http://dx.doi.org/10.15585/mmwr.mm6617a2. Accessed July 8, 2019.
-
8
Fleming JA, Dieye Y, Ba O, et al. Effectiveness of Haemophilus influenzae type B conjugate vaccine for prevention of meningitis in Senegal. Pediatr Infect Dis J. 2011;30(5):430-432. https://doi.org/10.1097/INF.0b013e318203aaa0. Accessed January 9, 2017.
-
9
WHO vaccine-preventable diseases: monitoring system. 2019 global summary. World Health Organization immunization data website. http://apps.who.int/immunization_monitoring/globalsummary/estimates?c=SEN. Accessed July 9, 2019.
-
10
GBD results tool. Institute for Health Metrics and Evaluation (IHME) website. Seattle, WA. http://ghdx.healthdata.org/gbd-results-tool. Accessed January 10, 2018.
-
11
Meningitis A vaccine support: Gavi’s response. Gavi, The Vaccine Alliance website. http://www.gavi.org/support/nvs/meningitis-a/. Accessed January 12, 2018.
-
12
Meningitis vaccine introduced in Africa’s meningitis belt. Gavi, The Vaccine Alliance website. http://www.gavi.org/library/news/statements/2010/meningitis-vaccine-introduced-in-africa-s-meningitis-belt/. Published December 6, 2010. Accessed July 3, 2019.
-
13
Ba F, Seck A, Bâ M, et al. Identifying an appropriate PCV for use in Senegal, recent insights concerning Streptococcus pneumoniae NP carriage and IPD in Dakar. BMC Infect Dis. 2014;14:627. https://doi.org/10.1186/s12879-014-0627-8. Accessed July 3, 2019.
-
14
GAVI Alliance welcomes introduction of two life-saving vaccines in Senegal. Gavi, The Vaccine Alliance website. http://www.gavi.org/library/news/statements/2013/gavi-alliance-welcomes-introduction-of-two-life-saving-vaccines-in-senegal/. Published November 5, 2013. Accessed July 3, 2019.
-
15
Gavi, The Vaccine Alliance. Advance Market Commitment for Pneumococcal Vaccines Annual Report 1 January - 31 December 2016. Geneva: Gavi; 2016. https://www.gavi.org/library/gavi-documents/amc/2016-pneumococcal-amc-annual-report/. Accessed July 9, 2019.
-
16
Senegal proposals, reports, and plans. Gavi, the Vaccine Alliance website. https://www.gavi.org/country/senegal/documents/. Accessed July 3, 2019.
-
17
Rotavirus vaccine support. Gavi, the Vaccine Alliance website. https://www.gavi.org/support/nvs/rotavirus/. Accessed December 20, 2018.
-
18
World Health Organization (WHO). Principles and Considerations for Adding a Vaccine to a National Immunization Programme: From Decision to Implementation and Monitoring. Geneva: WHO; 2014. http://apps.who.int/iris/bitstream/handle/10665/111548/9789241506892_eng.pdf;jsessionid=5E6C3DF8046BA8A504634EF46F9CDCD1?sequence=1. Accessed July 3, 2019.
-
19
Diop A, Thiongane A, Mwenda JM, et al. Impact of rotavirus vaccine on acute gastroenteritis in children under 5 years in Senegal: experience of sentinel site of the Albert Royer Children's Hospital in Dakar. Vaccine. 2018;36(47):7192-7197. https://doi.org/10.1016/j.vaccine.2017.10.061. Abstract accessed January 10, 2018
-
20
Senegal. Life-Saving Commodities Practitioners’ Network website. http://lifesavingcommodities.org/countries/senegal/. Accessed June 7, 2018.
-
21
Khan R, Vandelaer J, Yakubu A, Raza AA, Zulu F. Maternal and neonatal tetanus elimination: from protecting women and newborns to protecting all. Int J Womens Health. 2015;7:171–180. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4322871/pdf/ijwh-7-171.pdf. Accessed July 3, 2019.
-
22
Republic of Senegal Ministry of Public Health and Prevention. EPI Comprehensive Multiyear Plan; 2012–2016. Dakar: Republic of Senegal; 2011. http://www.gavi.org/Country/Senegal/Documents/CMYPs/Comprehensive-multi-year-plan-for-2012-2016/. Accessed July 3, 2019.
-
23
Tetanus protection at birth [Senegal]. STATcompiler. Rockville, MD: The DHS Program. https://www.statcompiler.com/en/. Accessed July 3, 2019.
-
24
Integrated Management of Childhood Illness. World Health Organization website. https://www.who.int/maternal_child_adolescent/topics/child/imci/en/. Accessed February 1, 2019.
-
25
Camara B, Faye PM, Diagne-Gueye NR, et al. [Evaluation of integrated management of childhood illness three years after implementation in a health care district in Senegal] (Article in French). Med Trop (Mars). 2008;68(2):162-166. https://www.ncbi.nlm.nih.gov/pubmed/18630049. Abstract accessed January 24, 2018.
-
26
Briggs J, Gabra M, Ickx P. Senegal Assessment: Drug Management for Childhood Illness. Arlington, VA: Management Sciences for Health, Rational Pharmaceutical Management Plus; 2002. https://www.researchgate.net/publication/237346394_SENEGAL_ASSESSMENT_DRUG_MANAGEMENT_FOR_CHILDHOOD_ILLNESS. Accessed July 3, 2019.
-
27
National Agency of Statistics and Demography (ANSD) [Senegal] and ICF. Sénégal: Enquête Démographique et de Santé Continue (EDS-Continue) 2016. Rockville, Maryland: ANSD and ICF; 2017; p. 134. https://dhsprogram.com/pubs/pdf/FR331/FR331.pdf. Accessed January 11, 2018.
-
28
President’s Malaria Initiative. Senegal Malaria Operational Plan FY 2015. Washington, DC: PMI; 2015. https://www.pmi.gov/docs/default-source/default-document-library/malaria-operational-plans/fy-15/senegal_mop_fy15.pdf?sfvrsn=4. Accessed December 24, 2018.
-
29
Physicians (per 1,000 people) and nurses and midwives (per 1,000 people). World Bank data site. https://data.worldbank.org/indicator/SH.MED.NUMW.P3?locations=SN. Accessed July 9, 2019.
-
30
Devlin K, Farnham Egan K, Pandit-Rajani T. Community Health Systems Catalog Country Profile: Senegal. Arlington, VA: Advancing Partners and Communities; 2016. https://www.advancingpartners.org/sites/default/files/catalog/profiles/senegal_chs_catalog_profile_0_0.pdf. Accessed July 9, 2019.
-
31
Jarrah Z, Wright K, Suraratdecha C, Collins D. Costing of Integrated Community Case Management in Senegal. Medford, MA: Management Sciences for Health, TRAction Project; 2013. https://www.msh.org/sites/msh.org/files/msh_costing_of_integrated_community_case_management_analysis_report_sene.pdf. Accessed July 3, 2019.
-
32
May highlights: updates from around the world. Sightsavers website. https://www.sightsavers.org/from-the-field/2018/05/may-highlights/. Published May 2018. Accessed July 9, 2019.
-
33
United States Agency for International Development (USAID) Maternal and Child Health Integrated Program (MCHIP). Review of Integrated Community Case Management Training and Supervision Materials in Ten African Countries. Washington, DC: USAID; 2013. https://www.mchip.net/sites/default/files/Report%20on%20Review%20of%20iCCM%20Training%20and%20Supervision%20materials.pdf. Accessed July 9, 2019.
-
34
Sylla A, Diouf S, Thiam A, et al. Assessment of the state and future of basic neonatal resuscitation equipment, in first-line health facilities in Senegal after 3 years. Archives de Pédiatrie. 2012;19(4), 355-360. https://doi.org/10.1016/J.ARCPED.2012.01.009. Accessed July 3, 2019.
-
35
Collins D, Jarrah Z, Gilmartin C, Saya U. The costs of integrated community case management (iCCM) programs: A multi–country analysis. J Glob Health. 2014;4(2):020407, p. 3. https://dx.doi.org/10.7189%2Fjogh.04.020407. Accessed January 10, 2018.
-
36
Daniels RF, Deme AB, Gomis JF, et al. Evidence of non-Plasmodium falciparum malaria infection in Kédougou, Sénégal. Malaria Journal. 2017;16:9. https://doi.org/10.1186/s12936-016-1661-3.
-
37
President’s Malaria Initiative. Senegal Malaria Operational Plan FY 2017. Washington, DC: PMI; 2017. https://www.pmi.gov/docs/default-source/default-document-library/malaria-operational-plans/fy17/fy-2017-senegal-malaria-operational-plan.pdf?sfvrsn=9. Accessed December 24, 2018.
-
38
WHO releases new guidance on insecticide-treated mosquito nets. World Health Organization website. https://www.who.int/mediacentre/news/releases/2007/pr43/en/. Published August 16, 2007. Accessed July 9, 2019.
-
39
Children under 5 who slept under an insecticide-treated net (ITN) [Senegal]. STATcompiler. Rockville, Maryland: The DHS Program. https://www.statcompiler.com/en/. Accessed July 3, 2019.
-
40
United States Agency for International Development (USAID). Malaria in Pregnancy Country Profile: Senegal. Washington, DC: USAID; 2018. https://www.mcsprogram.org/wp-content/uploads/dlm_uploads/2018/09/Senegal-MIPCountryProfile.pdf. Accessed July 9, 2019.
-
41
Cissé B, et al. Seasonal intermittent preventive treatment with artesunate and sulfadoxine-pyrimethamine for prevention of malaria in Senegalese children: a randomised, placebo-controlled, double-blind trial. The Lancet. 2006; 367(9511):659-667. https://doi.org/10.1016/S0140-6736(06)68264-0. Accessed July 3, 2019.
-
42
Bâ, E, Pitt C, Dial Y, et al. Implementation, coverage and equity of large-scale door-to-door delivery of Seasonal Malaria Chemoprevention (SMC) to children under 10 in Senegal. Scientific Reports. 2018;8:5489. https://doi.org/10.1038/s41598-018-23878-2. Accessed July 3, 2019.
-
43
Seasonal malaria chemoprevention. World Health Organization website. https://www.who.int/malaria/areas/preventive_therapies/children/en/. Updated May 1, 2017. Accessed July 9, 2019.
-
44
World Health Organization (WHO)/Global Malaria Program Technical Expert Group on Preventive Chemotherapy. Report of the Technical consultation on Seasonal Malaria Chemoprevention. Geneva: WHO; 2011. https://www.who.int/malaria/publications/atoz/smc_report_teg_meetingmay2011.pdf. Accessed July 9, 2019.
-
45
President’s Malaria Initiative. Senegal Malaria Operational Plan FY 2007. Washington, DC: PMI; 2006. https://www.pmi.gov/docs/default-source/default-document-library/malaria-operational-plans/fy07/senegal_mop-fy07.pdf?sfvrsn=6. Accessed December 24, 2018.
-
46
National Agency of Statistics and Demography (ANSD) [Senegal] and ICF International. Sénégal: Enquête Démographique et de Santé à Indicateurs Multiples Sénégal (EDS-MICS) 2010-2011. Calverton, Maryland: ANSD and ICF International; 2012; p. 194. https://dhsprogram.com/pubs/pdf/FR258/FR258_English.pdf. Accessed January 11, 2018.
-
47
National Agency of Statistics and Demography (ANSD) [Senegal] and ICF. Sénégal : Enquête Démographique et de Santé Continue (EDS-Continue) 2016. Rockville, Maryland: ANSD and ICF; 2017. https://dhsprogram.com/pubs/pdf/FR331/FR331.pdf. Accessed July 3, 2019.
-
48
Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease 2017. Seattle, WA: IHME; 2018. http://ghdx.healthdata.org/gbd-2017. Accessed July 3, 2019.
-
49
Victora C, et al. Analysis of Senegal DHS Survey Data. Brazil: International Center for Equity in Health, Federal University of Pelotas; 2018.
-
50
Quist-Arcton O. In Senegal, the grandmas are in charge. NPR. August 11, 2011. https://www.npr.org/2011/08/11/139543928/in-senegal-the-grandmas-are-in-charge. Accessed June 6, 2018.
-
51
Antenatal visits for pregnancy: 4+ visits (Three years preceding the survey) [Senegal]. STATcompiler. Rockville, MD: The DHS Program. https://www.statcompiler.com/en/. Accessed July 15, 2019.
-
52
Senegal triples number of people on HIV treatment. World Health Organization website. https://www.who.int/hiv/mediacentre/news58/en/. Published March 28, 2006. Accessed July 15, 2019.
-
53
Coverage of pregnant women who receive ARV for PMTCT [dataset] [Senegal]. UNAIDS website. http://aidsinfo.unaids.org/. Accessed July 15, 2019.
-
54
Baptiste DJ, Djibril D, Assane S, Ngagne M, Baly O, Ousmane N. Devenir sérologique et nutritionnel des nourrissons nés de mères séropositives suivis dans l’option B+ à Guédiawaye [Serological and nutritional outcome of infants born to HIV positive mothers undergoing option B + therapy in Guédiawaye]. Pan Afr Med J. 2016;25:224. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5337282/pdf/PAMJ-25-224.pdf. Accessed July 15, 2019.
-
55
AIDSinfo. UNAIDS website. http://aidsinfo.unaids.org/. Published 2018. Accessed May 30, 2019.
-
56
Siekmans K, Roche M, Kung’u JK, Desrochers RE, De-Regil LM. Barriers and enablers for iron folic acid (IFA) supplementation in pregnant women. Maternal Child Nutr. 2018;14(S5):e12532. https://doi.org/10.1111/mcn.12532. Accessed July 3, 2019.
-
57
Antenatal care content: Received iron tablets or syrup [Senegal]. STATcompiler. Rockville, Maryland: The DHS Program. https://www.statcompiler.com/en/. Accessed August 24, 2018.
-
58
National Agency of Statistics and Demography (ANSD) [Senegal] and ICF. Sénégal: Enquête Continue sur la Prestation des Services de Soins de Santé - ECPSS 2017. Rockville, Maryland: ANSD and ICF; 2018; p. 137. https://dhsprogram.com/pubs/pdf/SPA27/SPA27.pdf. Accessed July 15, 2019.
-
59
Ndiaye M, Siekmans K, Haddad S, Receveur O. Impact of a positive deviance approach to improve the effectiveness of an iron-supplementation program to control nutritional anemia among rural Senegalese pregnant women. Food Nutr Bull. 2009;30(2):128-136. https://doi.org/10.1177/156482650903000204. Accessed July 3, 2019.
-
60
Seck BC, Jackson RT. Determinants of compliance with iron supplementation among pregnant women in Senegal. Public Health Nutr. 2008;11(6):596-605. https://doi.org/10.1017/S1368980007000924. Abstract accessed January 15, 2018.
-
61
The Health Communication Capacity Collaborative. Demand Generation for 13 Life-Saving Commodities: A Synthesis of the Evidence. Baltimore, MD: Johns Hopkins Center for Communication Programs; 2014. http://sbccimplementationkits.org/demandrmnch/wp-content/uploads/sites/2/2015/04/Demand-Generation-A-Synthesis-of-the-Evidence-FINAL.pdf. Accessed July 3, 2019.
-
62
Helping Babies Breathe Global Development Alliance. Annual Status Report November 2013. 2013. https://www.healthynewbornnetwork.org/hnn-content/uploads/HBB-Annual-report-21-Nov-2013-Final_0.pdf.
-
63
Witter S, Bintou Drame F, Cross S. Maternal fee exemption in Senegal: is the policy a success? Afr J Midwifery Womens Health. 2009;3:5-10. https://doi.org/10.12968/ajmw.2009.3.1.39409. Accessed July 3, 2019.
-
64
Ravit M, Audibert M, Ridde V, et al. Removing user fees to improve access to caesarean delivery: a quasiexperimental evaluation in western Africa. BMJ Glob Health. 2018;3:e000558. https://doi.org/10.1136/bmjgh-2017-000558. Accessed July 3, 2019.
-
65
Witter S, Dieng T, Mbengue D, Moreira I, De Brouwere V. The national free delivery and caesarean policy in Senegal: evaluating process and outcomes. Health Policy Plan. 2010;25(5):384-392. https://doi.org/10.1093/heapol/czq013. Accessed July 3, 2019.
-
66
Witter S. Service- and population-based exemptions: are these the way forward for equity and efficiency in health financing in low-income countries? Adv Health Econ Health Serv Res. 2009;21:251-288. https://www.ncbi.nlm.nih.gov/pubmed/19791706. Accessed July 3, 2019.
-
67
Place of delivery: health facility [Senegal]. STATcompiler. Rockville, MD: The DHS Program. https://www.statcompiler.com/en/. Accessed April 26, 2019.
-
68
Children exclusively breastfed [0-5 months of age] [Senegal]. STATcompiler. Rockville, Maryland: The DHS Program.https://www.statcompiler.com/en/. Accessed July 3, 2019.
-
69
Faye PM, Thiongane A, Diagne-Gueye NR, et al. Les soins kangourou pour nouveau-nés de faible poids de naissance au centre hospitalier national d’enfants Albert-Royer de Dakar. [Kangaroo mother care for low birth weight infants at Albert-Royer National Children Hospital Center of Dakar]. Arch Pediatr. 2016;23(3):268-74. https://doi.org/10.1016/j.arcped.2015.12.010. Accessed July 3, 2019.
-
70
Senegal: A Leap Forward on Infant Survival. World Health Organization website. https://www.who.int/features/2013/senegal-infant-survival/en/. Published November 2013. Accessed July 3, 2019.
-
71
Ketsela T, Habimana P, Martines J, et al. Chapter 5: Integrated Management of Childhood Illness. In: Opportunities for Africa’s Newborns: Practical Data Policy and Programmatic Support for Newborn Care in Africa. Geneva: Partnership for Maternal and Child Health; 2006. http://www.who.int/pmnch/media/publications/aonsectionIII_5.pdf. Accessed July 3, 2019.
-
72
World Health Organization. Health workforce requirements for Universal Health Coverage and the Sustainable Development Goals. Geneva: World Health Organization; 2016. https://apps.who.int/iris/bitstream/handle/10665/250330/9789241511407-eng.pdf?sequence=1. Accessed April 25, 2019.
-
73
Gakidou, Emmanuela, et al. "Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2017." The Lancet 390.10100 (2017): 1345-1422. Institute for Health Metrics and Evaluation (IHME). Seattle, WA: IHME; 2018. Accessed Mar 2020.
