Why community was key in containing the 2022 mpox outbreak
Taking lessons from the HIV/AIDS epidemic, a focus on targeted outreach and a unified community response helped slow the outbreak
Deep into its third year battling the COVID-19 pandemic, the world found itself facing another global health emergency: the sudden spread of the rare mpox virus.
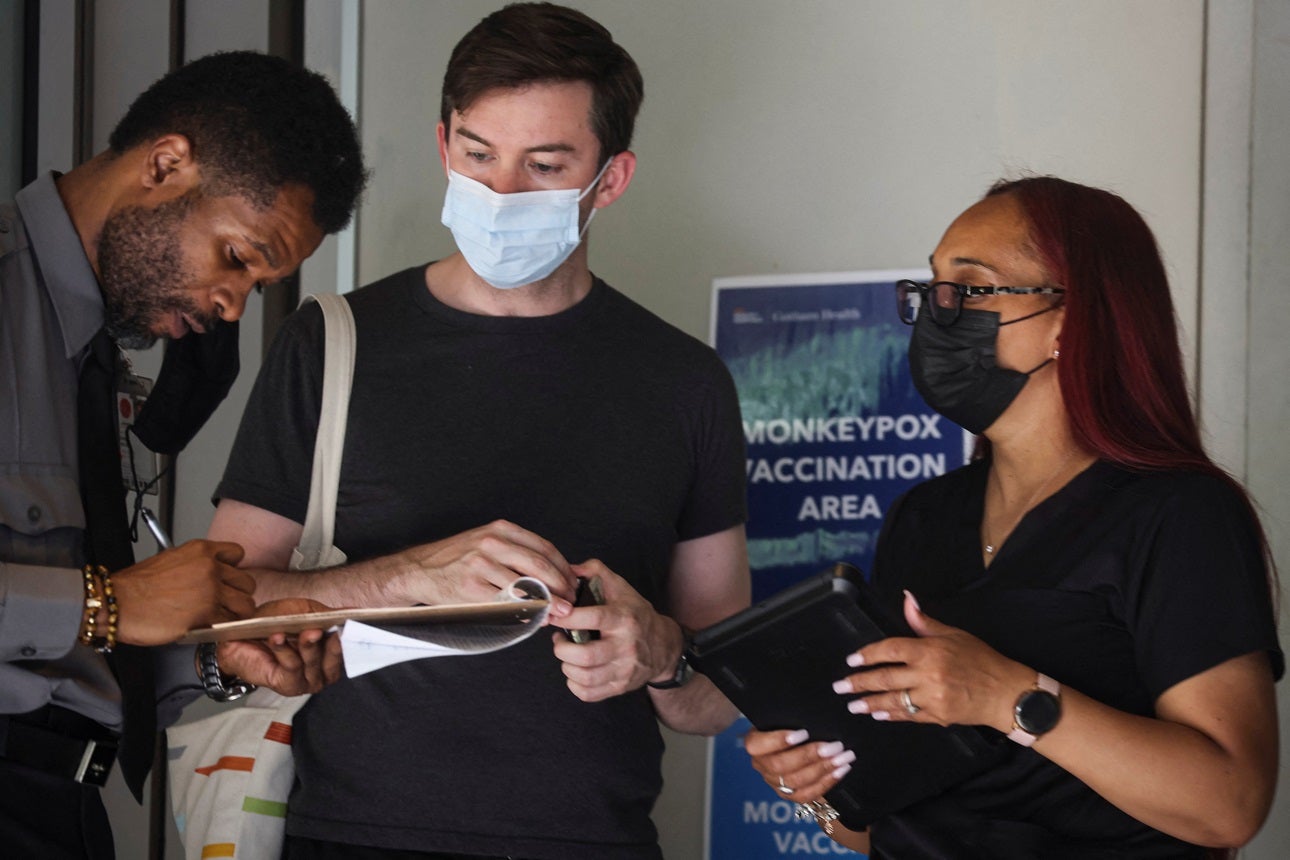
But, unlike with COVID, the outbreak of mpox – formerly called monkeypox – was contained in under a year, thanks to the rapid scaling of already available vaccines, targeted awareness campaigns, and a unified community response.
In May 2023, the World Health Organization announced that mpox was no longer a public health emergency of international concern. It had issued the emergency declaration in July 2022, after parts of Europe, Britain, the United States, Asia, and Australia started seeing alarming rates of the disease, which is normally seen in West and Central Africa.
Mpox, a less lethal cousin of smallpox, spreads through skin-to-skin contact or respiratory droplets. It can cause fever, headaches, swelling, aching muscles, and eventually painful lesions. Anyone can catch mpox, but in the latest outbreak, most of the confirmed cases outside of the regions in Africa where the disease is endemic were in gay, bisexual, or other men who have sex with men (MSM), almost half of them living with HIV.
It was lessons learned from the HIV/AIDS epidemic of the 1980s that drove many of the decisions governments and communities made in their response to the mpox outbreak. Authorities moved quickly to ramp up production and distribution of the vaccines JYNNEOS (also known by the brand names Imvamune or Imvanex) and ACAM2000, which – in another contrast to the COVID-19 pandemic – were already available.
Designed to protect against smallpox, the vaccines may be up to 85% effective in preventing mpox if used prior to exposure. Even if given between four and 14 days after exposure, they can still reduce symptoms of the disease.
The first mpox case in the latest outbreak was detected in London in early May 2022. Before the end of the month, a number of countries – including Britain, Germany, Spain, and the U.S. – had announced they were buying vaccines and/or releasing vaccines from their national stockpiles for domestic use and to send to other countries.
Many countries offered vaccinations to sexually active MSM, but the worry was that stigma around the disease would discourage many of those already marginalized groups from getting tested or seeking treatment, just as it did during the HIV/AIDS epidemic.
From early on in the mpox outbreak, public health efforts were aimed at encouraging gay, bisexual, and other men who have sex with men to reduce the number of their sexual partners and get tested and treated, while also raising awareness and debunking misinformation to combat discrimination against those groups.
At the same time, LGBTQ rights groups worked with officials and each other to help gay and bisexual men protect themselves from yet another disease that was threatening to ravage their community.
The groups issued statements to the media with guidance on how to cover the outbreak without stigmatizing the people who were most vulnerable to it. Community members encouraged each other to get vaccinated, using everything from online group chats to QR codes printed on napkins in gay bars to get the word out.
Top health officials, including those who made up the White House's newly formed National Monkeypox Response team, held regular meetings with LGBTQ organizations to collaborate on outreach and distribution of resources.
UNAIDS highlighted the importance of taking an evidence-based approach to the outbreak and reiterated that the spread of the disease was linked to behavior, not identity. The organization also lauded the LGBTQ community for leading the way in raising awareness of the disease, as community members.
“This outbreak highlights the urgent need for leaders to strengthen pandemic prevention, including building stronger community-led capacity and human rights infrastructure to support effective and non-stigmatizing responses to outbreaks,” said Matthew Kavanagh, UNAIDS Deputy Executive Director at the time, in a statement.
In June 2022, the WHO renamed the disease mpox to distance it from the stigma and racism associated with "monkeypox," a name that came from the lab monkeys that were first found to be carrying it in 1958.
The combination of targeted, socially sensitive outreach and speedy vaccine rollout seemed to get results. A survey of gay and bisexual men in the U.S. published in August 2022 showed about half of respondents had reduced their number of sexual partners or one-time sexual encounters to protect themselves and their partners from mpox.
As of May 5, 2023, more than 1.2 million vaccine doses had been administered in the U.S., which saw nearly a third of the world's mpox cases in the latest outbreak.
By the time the WHO declared an end to the public health emergency for mpox, more than 87,000 cases and 140 deaths had been reported from 111 countries, according to the organization's count, making it the largest ever global outbreak of the disease.
Although the emergency is over, the U.S. Centers for Disease Control and Prevention has warned that mpox cases could rise again over the summer as people gather together for parties and festivals.
All countries should "remain vigilant," the WHO Director-General Tedros Adhanom Ghebreyesus said in a press conference in May 2023. "Mpox continues to pose significant public health challenges that need a robust, proactive and sustainable response," he said. "While we welcome the downward trend of mpox cases globally, the virus continues to affect communities in all regions, including in Africa, where transmission is still not well understood."
How can we help you?
believes that the quickest path to improving health outcomes to identify positive outliers in health and help leaders implement lessons in their own countries.
With our network of in-country and cross-country partners, we research countries that have made extraordinary progress in important health outcomes and share actionable lessons with public health decisionmakers.
Our research can support you to learn about a new issue, design a new policy, or implement a new program by providing context-specific recommendations rooted in Exemplar findings. Our decision-support offerings include courses, workshops, peer-to-peer collaboration support, tailored analyses, and sub-national research.
If you'd like to find out more about how we could help you, please click . Please consider so you never miss new insights from Exemplar countries. You can also follow us on Twitter and LinkedIn.
